
What is Endometriosis?
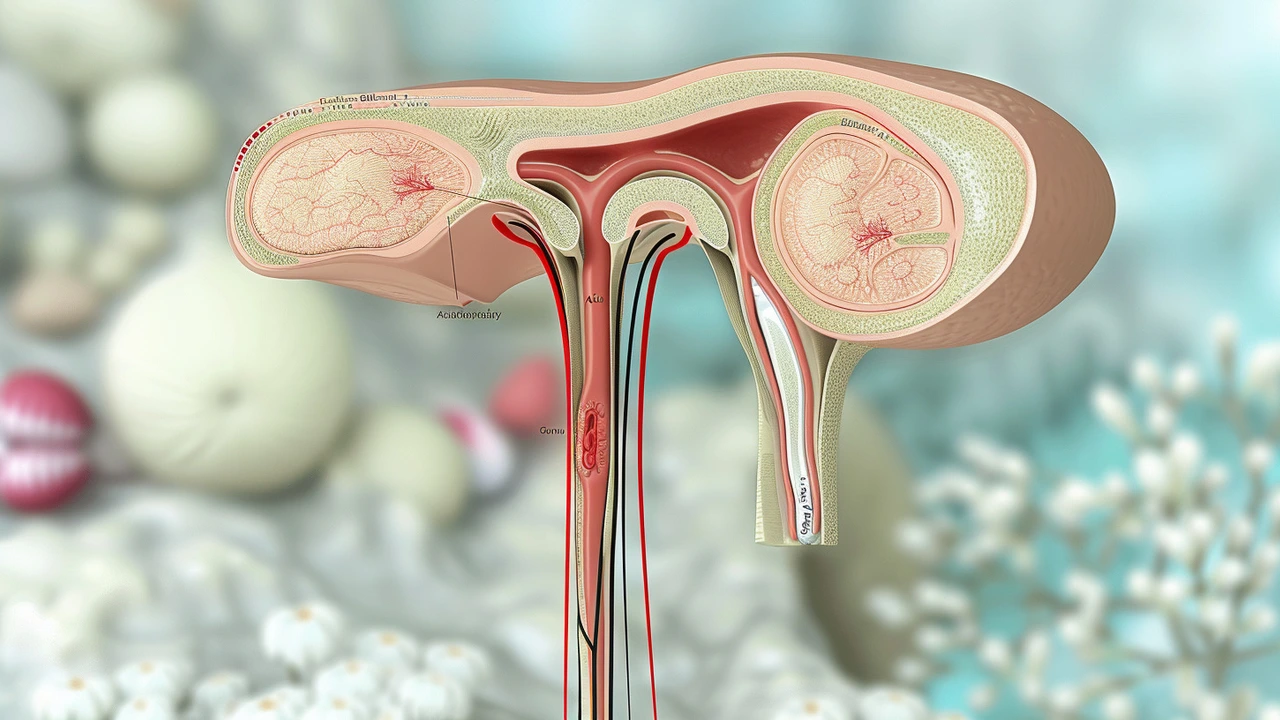
Endometriosis is a chronic disease that significantly impacts the lives of millions of women and girls worldwide. Characterized by the growth of endometrial-like tissue outside the uterus, it manifests in various symptoms that range from painful menstrual cycles to chronic pelvic pain and beyond. According to the World Health Organization (WHO), this condition affects approximately 10% of reproductive-age women and girls, translating to roughly 190 million individuals globally. Unlike the normal endometrial tissue that lines the uterus and sheds during menstrual cycles, the endometrial-like tissue outside the uterus causes severe complications. There is no known cure, making symptom management the primary focus of treatment.
The disease begins as early as the first menstrual period and can last until menopause, resulting in symptoms that can vary from mild to debilitating. The presence of this misplaced tissue causes inflammation, leading to pain, which can be particularly severe during menstrual cycles. Beyond menstrual pain, individuals also report pain during sexual intercourse, bowel movements, and urination. In addition to physical pain, endometriosis can result in significant emotional and psychological issues, including depression, anxiety, and infertility. The condition’s impact on daily life can therefore be profound and multifaceted.
Common Symptoms of Endometriosis
Among the most common and troubling symptoms of endometriosis is chronic pelvic pain, which can severely diminish the quality of life. Women often experience this pain during their menstruation cycles, and it can be so intense that it interferes with daily activities. Another prevalent symptom is heavy bleeding, either during or between periods. This can lead to secondary issues such as anemia, exacerbating feelings of fatigue and overall weakness.
Beyond pain and bleeding, endometriosis often presents a range of gastrointestinal and urological symptoms. These can include bloating, nausea, and pain during bowel movements, often leading to a misdiagnosis of gastrointestinal disorders initially. Painful urination is another marker that complicates the condition further. Fatigue is a frequent companion for those suffering from endometriosis, and it is compounded by physical pain and emotional stress. This fatigue can sometimes resemble chronic fatigue syndrome, making the condition even harder to diagnose correctly and promptly.
Psychological Impact
The emotional toll of endometriosis is undeniable. Chronic pain and the challenges it brings can lead to significant mental health issues, including depression and anxiety. The inability to predict when the pain will flare up adds to the stress, making planning and participating in activities challenging. Over time, the continual cycle of pain and fatigue can severely impact an individual's mental well-being and social life.
Additionally, infertility associated with endometriosis can deeply affect emotional health. The World Health Organization notes that about 30-50% of women with endometriosis may experience some form of infertility. This can lead to a complex emotional journey filled with stress, sadness, and in some cases, depression. The psychological effects thus amplify the physical symptoms, creating a vicious cycle that can be hard to break without comprehensive medical and psychological intervention.
Potential Causes of Endometriosis
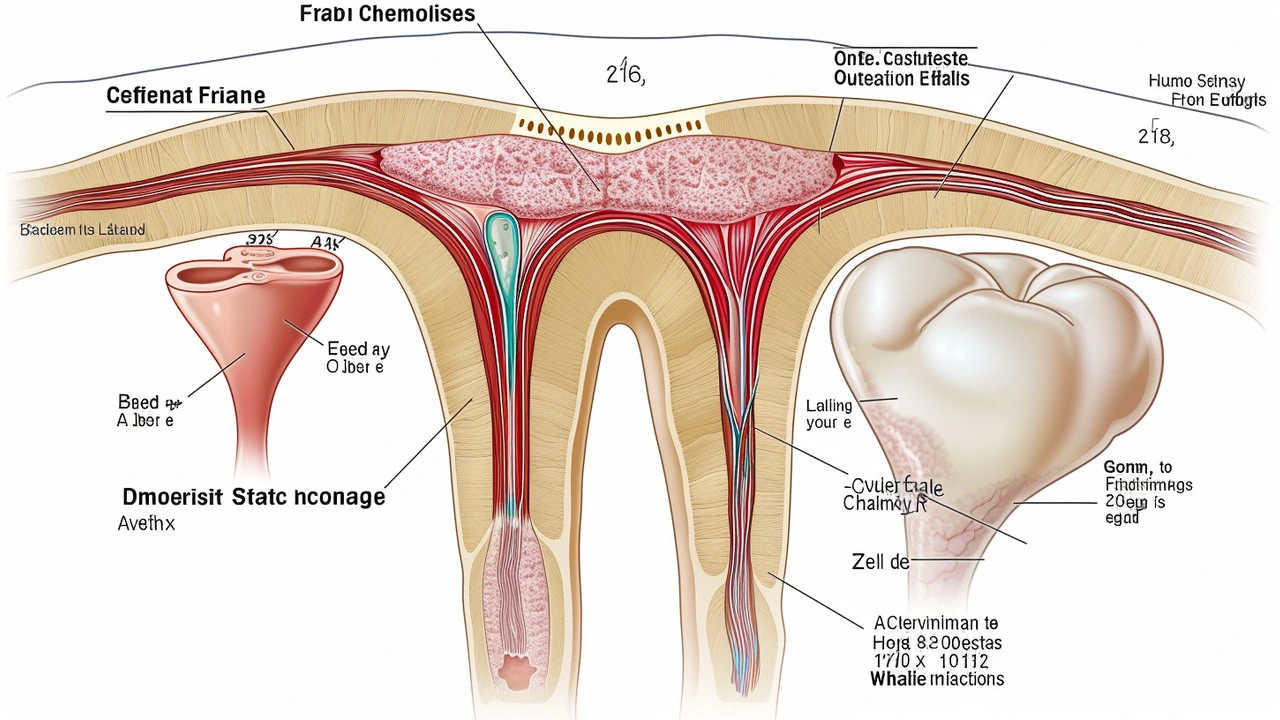
While the exact cause of endometriosis remains unknown, several theories provide insight into its possible origins. One of the earliest and most enduring theories is that of retrograde menstruation. This theory suggests that menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body. The cells in this menstrual blood then attach to pelvic organs and grow, causing the characteristic pain and symptoms of endometriosis.
Another theory posits cellular metaplasia, where cells located in different areas of the body transform into endometrial-like cells. Though less understood, this theory adds another layer of complexity to understanding the disease. Additionally, the role of stem cells has been explored, suggesting that stem cells in the bone marrow may contribute to the aberrant growth of endometrial-like tissue outside the uterus. Genetic factors are also considered to play a role, as women with a family history of endometriosis are often at a higher risk.
The hormonal environment plays a crucial role as well. Estrogen seems to promote the growth of endometrial tissue, making conditions that elevate estrogen levels likely contributors to the development and exacerbation of endometriosis. Understanding these potential causes aids in developing targeted treatments and therapies aimed at symptom management rather than a cure.
Social and Economic Implications
Endometriosis is not just a medical condition; it has extensive social and economic repercussions. Women with endometriosis often find themselves facing limitations in various aspects of life, from professional to personal. The chronic pain and fatigue can lead to decreased productivity at work, resulting in missed opportunities for career advancement and, in severe cases, loss of employment. Employers and healthcare systems bear significant costs due to the recurring medical interventions, managing chronic pain, and the resultant mental health issues.
The economic burden extends into healthcare costs. Frequent doctor visits, surgeries, and ongoing medication to manage pain and other symptoms can be financially draining. In countries where healthcare is not universally provided, these costs can become an insurmountable barrier to accessing adequate care. Furthermore, the economic burden is shared by families, who may also face emotional stress and financial instability stemming from medical expenses and caretaking responsibilities.
Management and Treatment Strategies
Since a cure for endometriosis remains elusive, treatment focuses on managing symptoms and improving the quality of life. Pain management typically involves medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and hormonal therapies to reduce menstrual flow and pain. For some, hormonal contraceptives help to minimize symptoms, but these treatments are not always effective and can have side effects.
In severe cases, surgical interventions might be considered. Laparoscopic surgery is often employed to remove endometrial tissue and can provide significant relief. However, surgery is not a permanent solution, as symptoms may recur. Regular follow-ups and a multi-disciplinary approach that includes gynecologists, pain specialists, and mental health professionals are often necessary.
Alternative Therapies
Many women turn to alternative therapies to manage their symptoms. Acupuncture, dietary changes, and exercise programs have shown some promise in alleviating symptoms. While these therapies may not replace conventional treatments, they can provide significant complementary benefits, improving overall well-being and quality of life.
Psychological support is equally critical. Counseling and support groups can provide emotional relief, helping individuals cope with the chronic nature of the disease and its impact on their lives. Cognitive behavioral therapy (CBT) has been particularly effective in managing the anxiety and depression that often accompany endometriosis.
Importance of Early Diagnosis
One of the most effective ways to manage endometriosis is through early diagnosis. Enhanced awareness and education about the symptoms of the disease can lead to prompt medical attention, slowing or halting the progression of the disease. Early intervention can significantly reduce the physical and emotional burden, enabling a more manageable quality of life.
Medical professionals are encouraged to consider endometriosis when diagnosing pelvic pain and other related symptoms, even in young girls just beginning their menstrual cycles. By adopting a proactive approach, including regular screenings and detailed patient history, doctors can identify and manage the disease more effectively, improving long-term outcomes for those affected.
A Global Perspective
Globally, the recognition of endometriosis as a significant public health issue is growing. Various organizations, including the World Health Organization, are advocating for increased research and funding to better understand the disease and develop more effective treatments. As awareness spreads, so does the push for policy changes to provide better support and resources for those afflicted by endometriosis.
Conclusion
Endometriosis is more than just a medical condition; it is a multifaceted issue that affects millions of women and girls worldwide. Chronic pain, emotional distress, and significant economic burdens characterize the lives of those living with the disease. Though current treatments focus on symptom management rather than a cure, ongoing research and increased awareness offer hope. Early diagnosis and a comprehensive, multi-disciplinary treatment approach are crucial to improving the quality of life for those affected. As more light is shed on this invisible illness, there is hope that future generations will face less stigma and more effective treatment for endometriosis.
Comments (17)
-
Chinmay Bhoot June 5, 2024
Another “miracle cure” hype, same old story.
-
Raj Bajoria June 6, 2024
Endometriosis is a real pain that affects so many women worldwide.
Early detection can change lives and reduce long‑term suffering.
-
Simardeep Singh June 6, 2024
When the body rebels, the mind often follows.
The chronic ache becomes a silent teacher about our fragility.
We end up negotiating with pain daily.
Understanding that dance can be oddly empowering.
-
Aryan Singh June 6, 2024
First off, the pharmacological arsenal includes NSAIDs, which are the frontline for managing menstrual‑related cramping.
Second, hormonal therapies such as combined oral contraceptives, progestins, and GnRH analogues work by suppressing ovulation and estrogen production, thereby limiting the growth of ectopic endometrial tissue.
Third, for women who cannot tolerate hormonal side‑effects, the levonorgestrel intrauterine system offers localized progestin release with minimal systemic impact.
Surgical options start with diagnostic laparoscopy, which not only confirms the diagnosis but also allows excision of visible lesions.
Laparoscopic excision or ablation can provide significant symptom relief, though recurrence rates remain notable, especially if deep infiltrating disease was present.
For extensive disease, a staged approach combining laparoscopic removal with postoperative hormonal suppression yields the best outcomes.
Pain clinics may incorporate neuromodulators, such as gabapentin or duloxetine, to address central sensitization that often accompanies chronic pelvic pain.
Physical therapy focusing on pelvic floor dysfunction can reduce myofascial pain components and improve quality of life.
Dietary interventions-low‑inflammatory diets rich in omega‑3 fatty acids, limited red meat, and high fiber-have anecdotal support and may help some patients.
-
Poorna Subramanian June 6, 2024
Stay strong keep pushing forward the journey may be tough but you’ve got this
-
Soundarya Kumar June 6, 2024
It’s crazy how something invisible can dominate every aspect of life.
Just know there’s a whole community out there rooting for you.
-
Sudaman TM June 7, 2024
Honestly, all this “holistic” talk is just a marketing ploy 🙄💊🤦♂️
-
Rohit Bafna June 7, 2024
The etiopathogenesis remains a paradigm of multifactorial interplay-retrograde menstruation, coelomic metaplasia, and stem‑cell dissemination converge under estrogenic milieu.
Epigenetic modifications further exacerbate lesion persistence.
Thus, any monotherapy is inevitably suboptimal.
-
Minal Chavan June 7, 2024
Endometriosis carries substantial socioeconomic ramifications.
Policy interventions are essential to alleviate the burden.
-
Rajesh Soni June 7, 2024
Oh sure, just another “miracle” diet plan that will fix everything.
We’ve seen that one before.
-
Nanda Dyah June 7, 2024
Inasmuch as evidence suggests, clinical management must be both multidisciplinary and patient‑centered.
The integration of gynecologic, pain‑specialist, and mental‑health expertise yields optimal outcomes.
Failure to adopt such an approach constitutes a dereliction of duty.
Therefore, systemic reform is warranted.
-
vikas duhun June 8, 2024
This is the tragedy of a silent war raging inside women’s bodies!
Enough is enough!
-
Nathan Rodan June 8, 2024
Let’s keep sharing resources and support each other.
Together we can push for better research funding.
Every voice matters.
-
KABIR SETHI June 8, 2024
Did you know that deep infiltrating endometriosis can affect the bowel and bladder?
It’s often misdiagnosed as IBS or urinary tract infection.
Awareness is the first step.
-
rudal rajbhar June 8, 2024
Philosophically, the pain is a reminder of the body’s revolt against oppressive hormonal hierarchies.
We must confront this reality with scientific rigor and unflinching resolve.
Idle sympathy will not cure the disease.
-
tanay bole June 8, 2024
The data clearly indicate a need for earlier diagnostic protocols.
Clinicians should be vigilant.
-
Darrell Kuykendall June 9, 2024
Wow! This is such an informative overview! Keep spreading the word!!!
